Survival of jak inhibitors: real-word data from the biobadaser III registry

Visualización o descarga de ficheros
Visualización o descarga de ficheros
Fecha de publicación
2019Título de revista
Annals of the rheumatic diseases
Tipo de contenido
Publicación de congreso
Resumen
Background JAK inhibitors (JAKi) have been recently authorized in the European Union. JAKi long-term performance in the clinical practice setting still needs to be assessed. Drug survival reflects a drug’s effectiveness, safety, and tolerability; thus, it is an important measurement for real-world studies.
Objectives To describe the pattern of use of JAKi in real-world dataset, and to analyze the drug survival as a group (tofacitinib+baricitinib).
Methods Information was obtained from BIOBADASER III, an ongoing observational longitudinal multicenter cohort of patients with rheumatic diseases treated with biologic or targeted synthetic (b/ts) DMARDs in Spain. All subjects with current or previous JAKi use were included and followed until September 2018. Clinical characteristics of the patients were analyzed. Drug survival (overall, and for biologic-naive and biologic-experienced patients) was determined using Kaplan-Meier analysis.
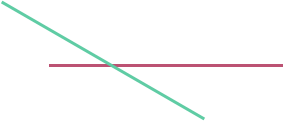
Results 149 patients, 75.2% women, were treated with JAKi, receiving a total of 152 cycles of treatment (50.7% tofacitinib, 49.3% baricitinib; 3 patients had both). The most frequent diagnosis was rheumatoid arthritis (RA, 92.6%), and there is a small number of off-label uses (6%), depicted at Table 1. Use on psoriatic arthritis is scarce (1.3%). Concomitant use of methotrexate (MTX) was registered in 68 patients (45.6%). Previous use of bDMARDs was high (n=124, 81.6%); drug survival rate for biologic-experienced patients was 81.7% and 78.7% at 6 and 12 months. None of the JAKi treatments in biologic-naive patients (n=18, 18.4%) were discontinued during follow-up. Pooled survival rate of JAKi was 85.0% and 82.5% at 6 and 12 months (Figure 1). Discontinuation was seen in 19 treatments (12.5%); the reasons were inefficacy (n=15, 9.9%) or adverse events (n=4, 2.6%).
Conclusion The current use of JAKi in Spain is mainly in RA and as 2nd line after bDMARDs. The use of JAKi in psoriatic arthritis is still scarce and a small group of patients are treated off-label. Less than half use combination therapy with MTX. Overall survival of JAKi is superior to 80% at 12 months. A longer follow-up is needed to continue analyzing the survival of JAKi in a real-world context.